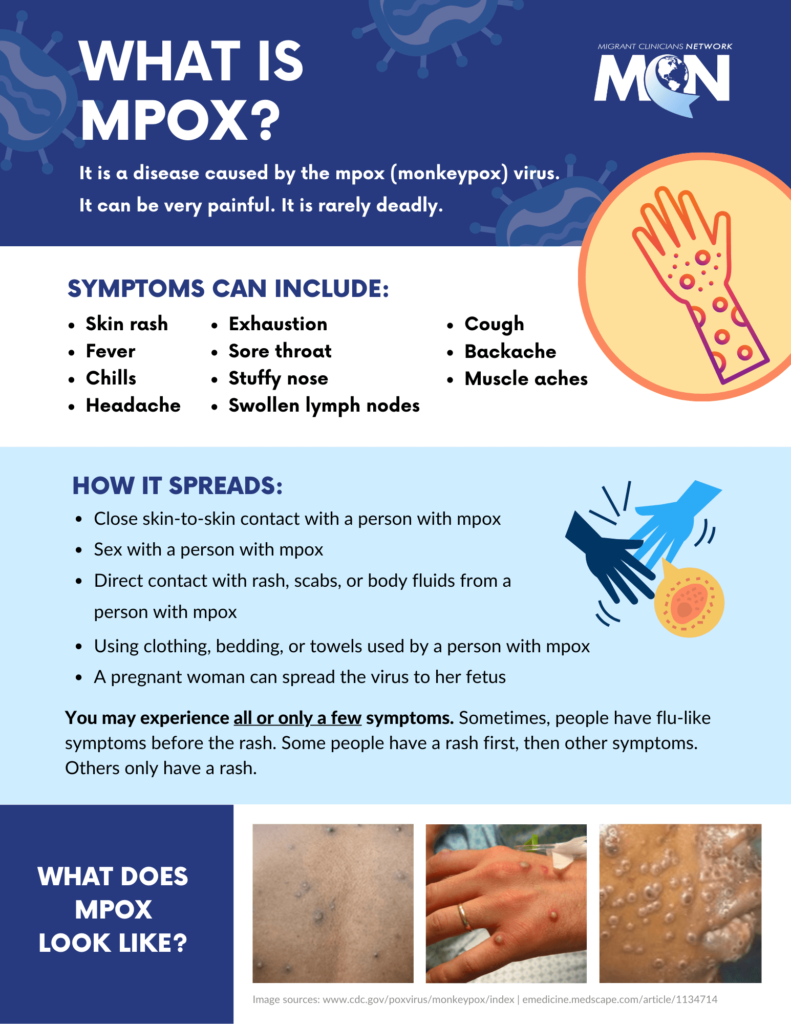
What is Mpox?
Mpox, formerly known as monkeypox, is a viral zoonotic disease caused by the mpox virus, a member of the Orthopoxvirus genus in the family Poxviridae. It was first discovered in 1958 in monkeys kept for research, and the first human case was recorded in 1970 in the Democratic Republic of the Congo. The virus is closely related to the smallpox virus, although mpox is generally less severe.
Is Mpox the Same as Chickenpox?
No, mpox is not the same as chickenpox. Although both diseases cause rashes and can appear similar, they are caused by different viruses and have distinct characteristics:
- Mpox: Caused by the mpox virus, which belongs to the Orthopoxvirus genus. It is related to the smallpox virus, and the symptoms are more severe than those of chickenpox. Mpox often involves swollen lymph nodes, which is not a common feature of chickenpox.
- Chickenpox: Caused by the varicella-zoster virus (VZV), a member of the herpesvirus family. Chickenpox is generally milder and primarily affects children, although adults can also contract it.
Can Someone Who Had Chickenpox Still Get Mpox?
Yes, someone who has had chickenpox can still get mpox. Immunity to chickenpox does not provide immunity to mpox because they are caused by entirely different viruses. Having had chickenpox or receiving the chickenpox vaccine does not protect against mpox infection. This is an important distinction, especially for those who might assume they are immune to mpox because they had chickenpox in the past.
Mpox Strains and Clades
The mpox virus is divided into two distinct genetic clades:
- Clade I (Central African or Congo Basin Clade):
- This clade is primarily found in the Congo Basin and is known to cause more severe disease with a higher mortality rate (up to 10%).
- It has been historically more virulent and is capable of human-to-human transmission, though such transmission is still relatively uncommon.
- Clade II (West African Clade):
- This clade is found mainly in West Africa and has been responsible for most of the recent global outbreaks.
- The disease caused by this clade tends to be milder, with a lower mortality rate (around 1-3%).
- The West African clade is also less transmissible between humans compared to the Central African clade.
Recent outbreaks outside of Africa have predominantly involved the West African clade (Clade II), which is associated with milder symptoms and a lower mortality rate. However, due to the global movement of people and goods, the risk of the virus spreading remains significant.
Who is Most at Risk?
While anyone can contract mpox, certain groups are at higher risk of severe illness:
- People with Weakened Immune Systems: Individuals with compromised immune systems, including those with HIV/AIDS, cancer patients undergoing chemotherapy, and organ transplant recipients, are at higher risk of severe complications.
- Children: Young children, particularly those under the age of 8, are more vulnerable to severe illness from mpox.
- Pregnant Women: Pregnant women are at higher risk of complications, including potential risks to the unborn child.
- Healthcare Workers: Due to their exposure to infected individuals, healthcare workers are at increased risk, particularly if proper personal protective equipment (PPE) is not used.
- People in Close Contact with Infected Individuals: Household members and sexual partners of someone with mpox are at higher risk of contracting the virus.
Can Mpox Be Treated?
Mpox is generally a self-limiting disease, meaning it often resolves on its own without specific treatment. However, supportive care is crucial in managing symptoms and preventing complications. For severe cases or those at higher risk of complications, antiviral treatments such as Tecovirimat (TPOXX) may be used, though its availability might be limited. Additionally, healthcare providers may treat bacterial infections if they occur as a result of scratching or other complications.
Is Mpox Covered by PhilHealth?
Yes, as of the latest updates, PhilHealth covers the treatment of mpox under its infectious disease packages. The coverage includes hospitalization and necessary medical interventions, depending on the severity of the disease and the treatment required. Patients should consult with their healthcare provider and PhilHealth to understand the extent of coverage available to them.
Is Mpox Usually Covered by HMOs?
Coverage of mpox by Health Maintenance Organizations (HMOs) in the Philippines may vary depending on the HMO provider and the specific plan. Generally, HMOs cover outpatient consultations, diagnostics, and hospitalization for infectious diseases, including mpox, but it is essential to check with your specific HMO provider for detailed information on what is included in your plan.
Signs and Symptoms of Mpox
Mpox symptoms typically appear within 7 to 14 days after exposure to the virus but can range from 5 to 21 days. The illness usually lasts 2 to 4 weeks. The progression of symptoms generally occurs in the following stages:
- Prodromal Stage (Early Symptoms):
- Fever: A sudden rise in body temperature is one of the first signs.
- Headache: Persistent headaches are common during this stage.
- Muscle Aches: Myalgia, or muscle pain, often accompanies the fever.
- Backache: Many patients report significant back pain.
- Swollen Lymph Nodes (Lymphadenopathy): Unlike smallpox, mpox often causes noticeable swelling of the lymph nodes, particularly in the neck, armpits, and groin. This symptom helps distinguish mpox from other similar infections.
- Chills: Patients may experience shivering or chills as the fever develops.
- Exhaustion: A general feeling of fatigue and weakness is common.
- Rash Development (1-3 Days After Fever Onset):
- The rash typically begins on the face before spreading to other parts of the body, including the palms of the hands and soles of the feet.
- Macules: The rash starts as flat, red spots.
- Papules: These spots then become raised bumps.
- Vesicles: The bumps fill with clear fluid, turning into blisters.
- Pustules: The vesicles then fill with pus, which is a hallmark of mpox.
- Scabs: Eventually, the pustules crust over and scab. These scabs then fall off as the skin heals.
The rash usually follows this progression over the course of 2 to 4 weeks. In some cases, the lesions can be painful and may leave scars. The number of lesions can vary, with some individuals having just a few while others develop thousands.
Why Should You Worry About Mpox?
Recently, there have been reported cases of mpox in the Philippines. While mpox is not as contagious as COVID-19, it can spread from person to person through close contact, including:
- Direct contact with mpox sores, scabs, or body fluids.
- Respiratory droplets from prolonged face-to-face interaction.
- Touching contaminated items, such as bedding or clothing.
Statistics and Current Situation
- Global Context: Since the resurgence of mpox, over 86,000 cases have been reported globally, with significant outbreaks in non-endemic countries.
- Philippines: As of the latest reports, the Philippines has seen a handful of cases. The Department of Health (DOH) has been vigilant in monitoring and controlling the situation, but given the virus’s potential for spread, especially in densely populated areas, it is crucial for organizations to be proactive.
First Aid Options for Mpox
While mpox is generally a self-limiting disease, meaning it resolves on its own without specific treatment, supportive care can help alleviate symptoms and prevent complications. Here are first aid measures and supportive care options for individuals suspected of or diagnosed with mpox:
- Isolate the Patient:
- Immediate Isolation: If mpox is suspected, the patient should be isolated from others to prevent the spread of the virus. Ideally, the individual should stay in a separate room with its own bathroom.
- Use of PPE: Caregivers should wear personal protective equipment (PPE), including gloves, masks, and gowns, when handling the patient or their belongings.
- Symptomatic Relief:
- Fever and Pain Management: Use over-the-counter medications such as acetaminophen (paracetamol) or ibuprofen to manage fever, headaches, and muscle aches. Always follow the dosage instructions on the medication label.
- Hydration: Encourage the patient to drink plenty of fluids to stay hydrated. Dehydration can worsen symptoms and prolong recovery time.
- Care of Skin Lesions:
- Avoid Scratching: Scratching the lesions can lead to secondary bacterial infections. Keep the patient’s nails trimmed, and consider using gloves to minimize the risk.
- Topical Treatments: Apply antiseptic creams or ointments to the lesions to prevent bacterial infections. Calamine lotion may also be used to soothe itching.
- Cleanliness: Keep the affected skin clean and dry. Gently wash the lesions with soap and water, then pat them dry with a clean towel.
- Managing Respiratory Symptoms:
- Respiratory Isolation: If the patient exhibits respiratory symptoms (e.g., coughing, sneezing), ensure they wear a mask to prevent the spread of respiratory droplets.
- Ventilation: Keep the patient’s room well-ventilated to reduce the concentration of airborne virus particles.
- Monitor for Complications:
- Seek Medical Attention: If the patient experiences difficulty breathing, chest pain, confusion, or seizures, seek emergency medical care immediately.
- Monitor Vital Signs: Regularly monitor the patient’s temperature, heart rate, and breathing. Any significant changes should prompt a consultation with a healthcare provider.
- Safe Disposal of Contaminated Items:
- Disposal of Waste: Dispose of used tissues, bandages, and other contaminated items in a sealed plastic bag before placing them in the trash.
- Laundry Precautions: Wash the patient’s clothing, bedding, and towels separately from other household laundry. Use hot water and a strong detergent.
- Communication with Healthcare Providers:
- Report Symptoms: If a patient develops symptoms consistent with mpox, contact a healthcare provider for guidance on testing and further care.
- Follow-up Care: Patients diagnosed with mpox should have regular follow-ups with their healthcare provider to monitor recovery and manage any complications.
How to Avoid Mpox: Key Preventive Measures
- Vaccination: The smallpox vaccine has been shown to be 85% effective in preventing mpox. In some countries, targeted vaccination campaigns are being implemented.
- Personal Hygiene: Regular handwashing with soap and water or the use of alcohol-based hand sanitizers is essential.
- Avoid Close Contact: Limit close contact with individuals showing symptoms, such as rashes or lesions.
- Safe Handling of Items: Avoid touching personal items that have been used by someone with mpox. If necessary, handle them with gloves and wash them thoroughly.
- Awareness and Education: Stay informed about the symptoms and spread of mpox through credible sources like the World Health Organization (WHO) and local health authorities.
HR Measures to Protect Your Workplace
- Health and Safety Protocols: Update workplace health and safety protocols to include guidelines specific to mpox. This includes symptom screening, reporting, and isolation measures.
- Remote Work Options: For employees who are exposed or show symptoms, offer remote work options to prevent workplace transmission.
- Education and Training: Provide training sessions for employees on mpox prevention, symptoms, and response protocols.
- Sanitization Procedures: Increase the frequency of cleaning and disinfecting common areas, particularly surfaces that are frequently touched.
- PPE and Hygiene Supplies: Ensure that personal protective equipment (PPE) and hygiene supplies (e.g., hand sanitizers, gloves) are readily available to employees.
- Communication Strategy: Establish a clear communication plan for informing employees about mpox cases and preventive measures without causing unnecessary panic.
- Leave Policies: Review and update sick leave policies to support employees who may need to isolate or recover from mpox.
Conclusion
Mpox, though less severe than other viral infections, poses a significant risk, especially in a workplace setting. By understanding the disease, staying informed about its spread, and implementing robust HR measures, organizations can protect their employees and prevent disruption to business operations.
Becoming an Expert
International HR Institute provides global certification programs for modern-day HR professionals. Understand how you can implement robust HR measures to protect your employees by taking the Certified Practitioner in Human Resources certification program.